Description:
A 76 year old female presented with severe jaundice and itching associated with intractable vomiting for last 10 days. Patient had been diagnosed by us as a case of adenocarcioma of pancreatic head and uncinate process on Endoscopic ultrasound (EUS) guided FNB and EUS evaluation suggesting the tumor to be invading into the duodenum as well as the SMV-portal vein confluence, rendering it inoperable, three months back.
A repeat endoscopic evaluation on this visit revealed the tumor to be invading the D1-D2 junction, causing gastric outlet obstruction. Balloon dilatation of the stricturous duodenal segment was performed so as to rail road the duodenoscopeover the guidewire into the second part of duodenum.
Endoscopic retrograde cholangiogram(ERC) revealed bile duct obstruction in the intra-pancreatic part of CBD with dilated upper CBD. In view of these findings and inoperable nature of the disease, a self expandable 8 cm uncovered metallic billiary stent and a self expandable uncovered 14cm pyloro-duodenal metallic stent was placed as a means of palliation. Patient was completely relieved of the symptoms of bile duct obstruction as well as gastric outlet obstruction in three days.
Expert Comments
Almost 85% of patients of pancreatic cancer are deemed unsuitable candidates for curative resection at the time of diagnosis. Obstructive jaundice occurs in 70-80% of such patients and approximately 5% patients develop duodenal obstruction at some point before their death. Patients who require relief of bileduct obstruction and are not candidates for possible curative resection, it has been a standard of care to perform endoscopic stent placement.
Meta-analyses comparing enteral stent placement with gastro-jejunostomy have confirmed the high technical and clinical success rates of stent placement and indicated favorable outcomes with pyloro duodenal stenting.Endoscopy provides Detection, Diagnosis, Staging with EUS & FNA followed by palliation through ERCP with Metal Biliary Stenting and Pyloro-Duodenal Stenting.
If there duodenal narrowing that does not allow ERCP then we can always plan an EUS guided biliary drainage, so for the last almost 10 years we have obviated the need for PTC due to EUS guided biliary drainage option.
Take Home Message:
In view of more patients presenting in poor nutritional and general health status, intolerability to surgical stress and relatively short expected survival, self expandable metallic stents provide an attractive alternativeto palliative surgical intervention.
However, careful evaluation of the patient and procedural expertise are required for predictable post-procedural outcome. At Endoscopy Asia this protocol of EUS-ERCP-Endotherapy for such advanced inoperable pancreatic cancer palliation has been practiced for over 13 years.
We feel that Surgical Palliation of such a problem can be obviated in almost all the cases leading to either cholestatic or gastric outlet obstructive symptoms.
Image:
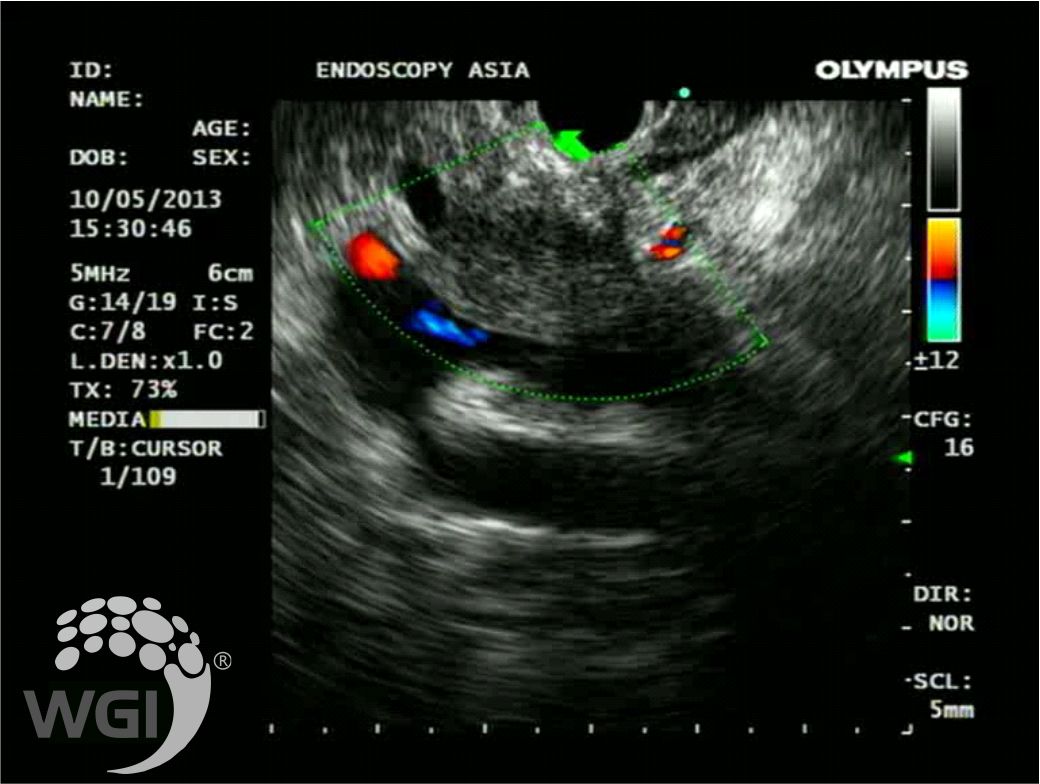
1. Mass in the Head of Pancreas encasing SMV-Portal Vein confluence
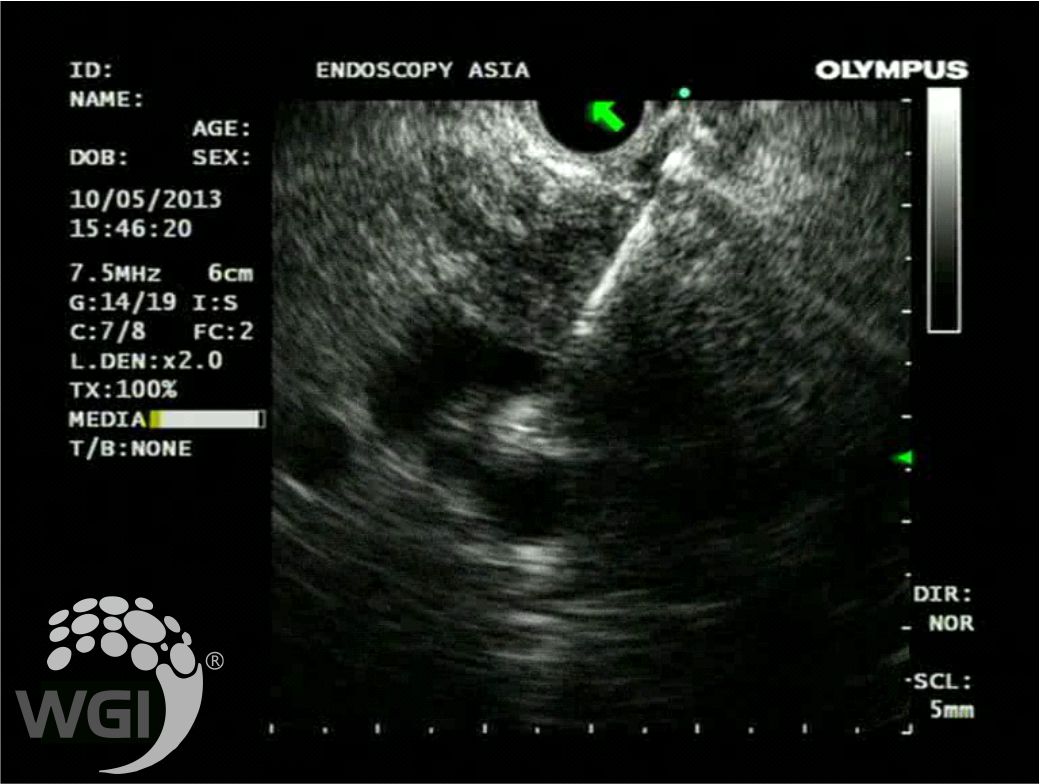
2. EUS guided FNA of the Pancreatic Head Mass
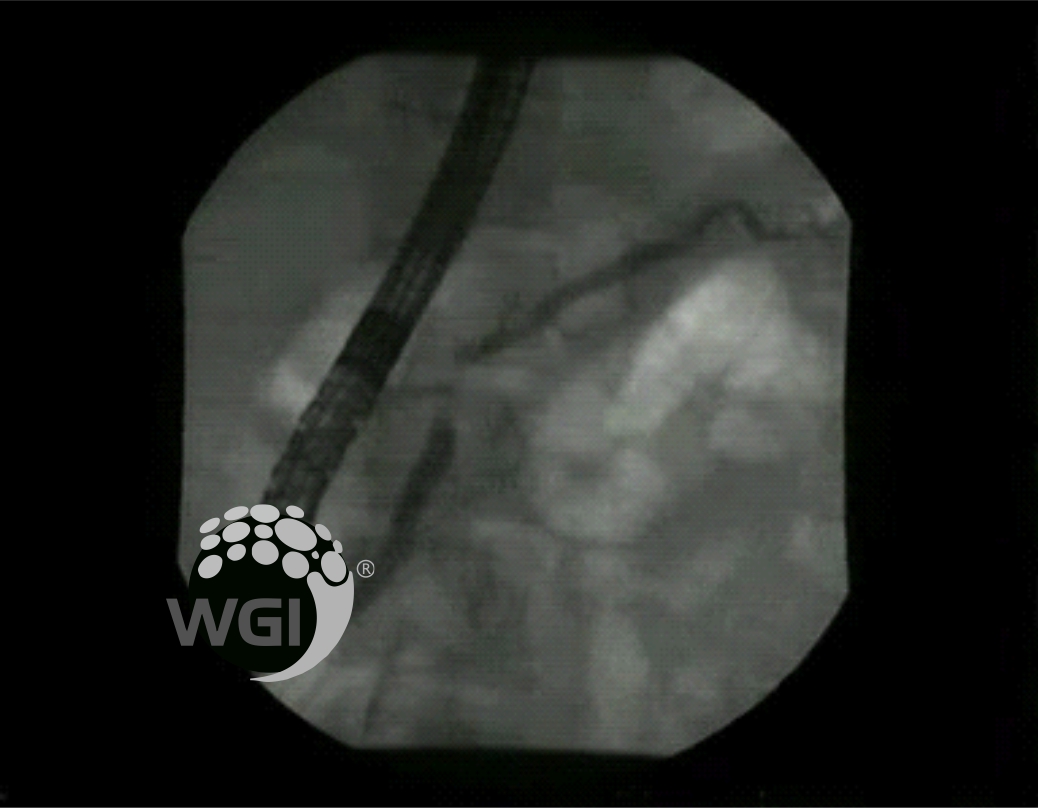
3. Cholangiogram showing Obstruction at Lower end of CBD with Proximal CBD Dilatation
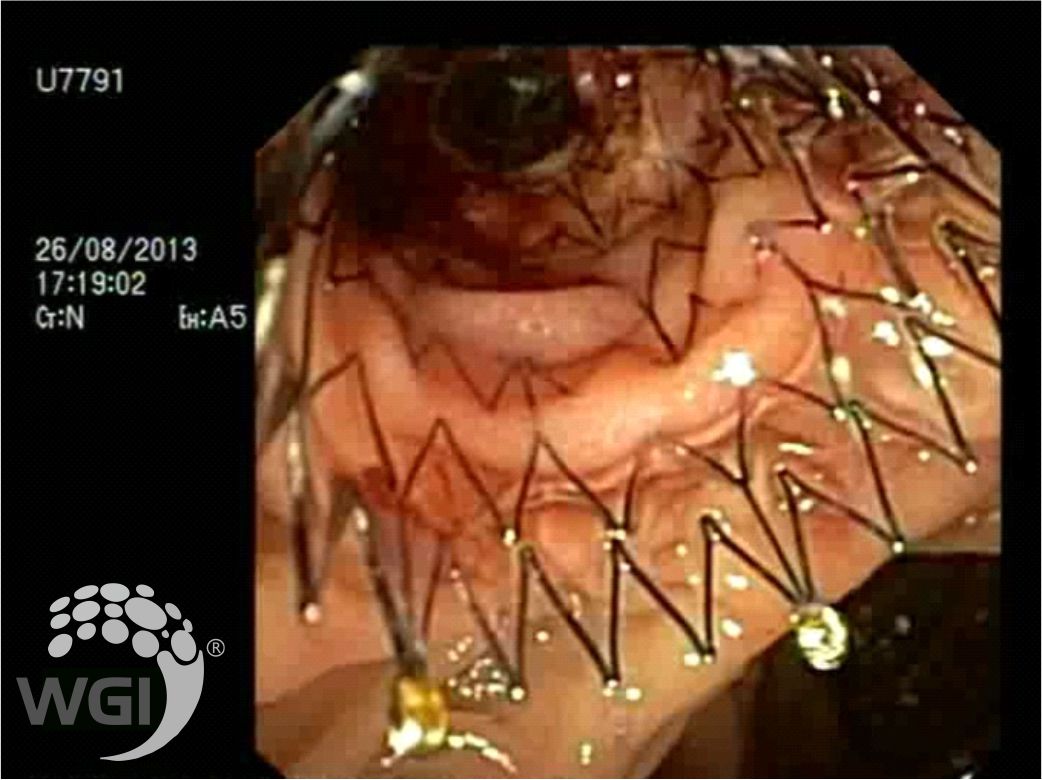
4. Self expandable biliary metallic stent in-situ
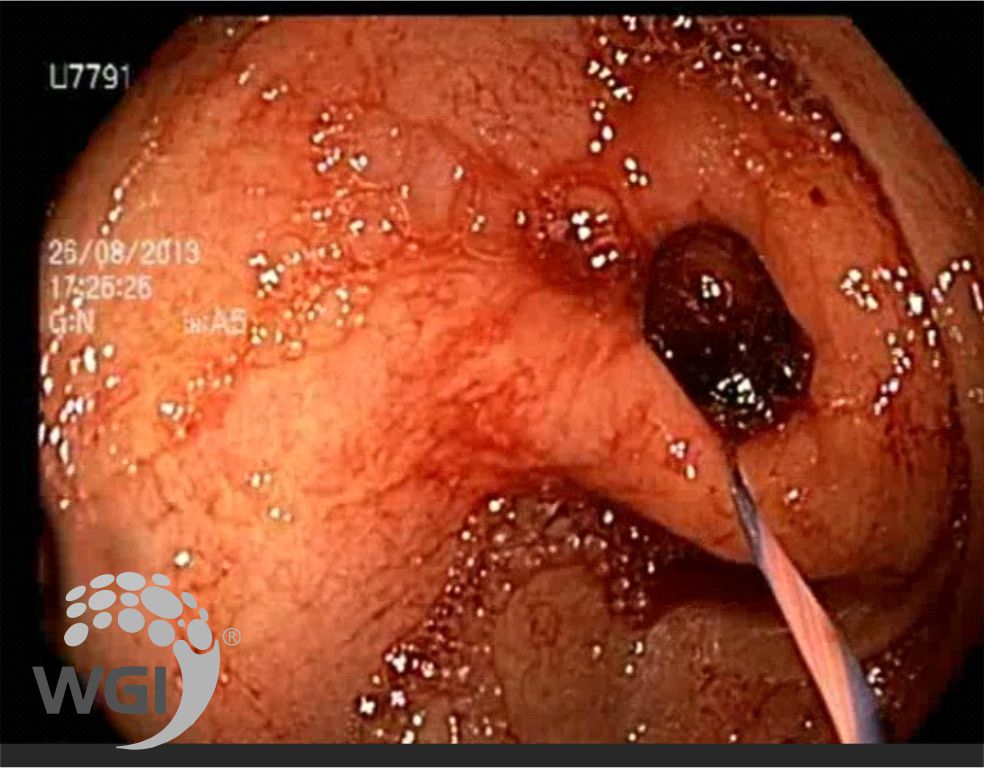
5. Guide wire in-situ across the Stricturous duodenal segment
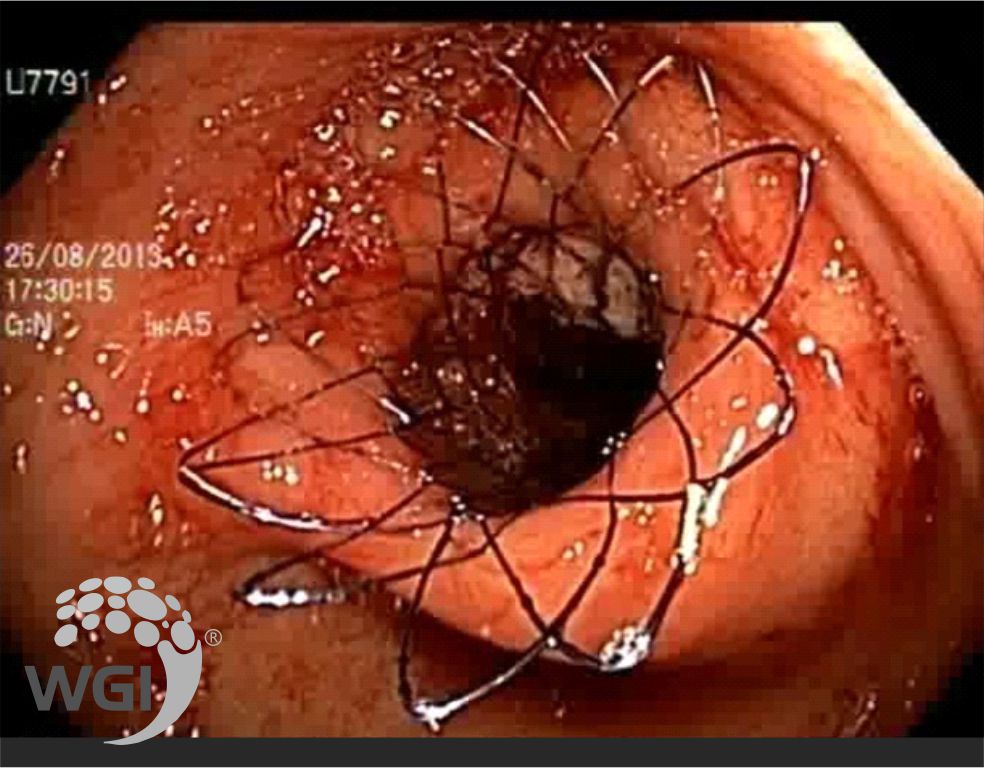
6. Self expandablePyloro-Duodenal Metallic stent in-situ